Introduction
Diabetes is a complex and prevalent health condition that affects millions of individuals worldwide. It is crucial to have a comprehensive understanding of diabetes to manage and prevent its complications effectively. In this article, we will explore diabetes in detail, covering its types, causes, symptoms, risk factors, diagnosis, treatment options, and prevention strategies.
Types of Diabetes
Type 1 Diabetes
Type 1 diabetes, often referred to as juvenile diabetes, is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This results in little to no insulin production. It typically develops in childhood or early adulthood and requires lifelong insulin therapy for blood sugar regulation.
Type 2 Diabetes
Type 2 diabetes is the most common form of diabetes, accounting for the majority of cases. It primarily affects adults but can occur in individuals of any age. In Type 2 diabetes, the body becomes resistant to insulin, or it does not produce enough insulin to maintain normal blood sugar levels. Lifestyle factors such as obesity, poor diet, and lack of exercise play a significant role in its development.
Gestational Diabetes
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased demands. While it often resolves after childbirth, women who have had gestational diabetes are at a higher risk of developing Type 2 diabetes later in life.
Type 1 Diabetes:
Introduction
Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition that affects approximately 5-10% of all individuals diagnosed with diabetes. It is distinct from Type 2 diabetes in terms of its causes, onset, and treatment. Understanding the intricacies of Type 1 diabetes is essential for those living with the condition, their caregivers, and the broader community.
The Basics
Insulin Production and Its Role
Insulin is a hormone produced by the pancreas. Its primary role is to regulate blood sugar (glucose) levels in the body. When we eat, our digestive system breaks down carbohydrates into glucose, which enters the bloodstream. In response, the pancreas releases insulin to allow cells to absorb glucose for energy. In Type 1 diabetes, this process is disrupted.
Causes of Type 1 Diabetes

Autoimmune Destruction of Beta Cells
Type 1 diabetes is fundamentally an autoimmune disease. It occurs when the body’s immune system mistakenly identifies and attacks healthy insulin-producing beta cells in the pancreas. The exact cause of this autoimmune response remains unknown, but genetic predisposition and environmental triggers are believed to play significant roles.
Genetic Predisposition
There is a strong genetic component to Type 1 diabetes. Individuals with a family history of the condition have a higher risk of developing it. Certain genes linked to the immune system are associated with an increased susceptibility.
Environmental Factors
While genetics may set the stage, environmental factors can trigger the autoimmune response leading to Type 1 diabetes. These factors may include viral infections during childhood, exposure to certain dietary factors, and other, as yet unidentified, triggers.
Onset and Symptoms
Rapid Onset
Type 1 diabetes often has a rapid onset, with symptoms appearing over a short period. This is in contrast to Type 2 diabetes, which usually develops more gradually.
Common Symptoms
The most common symptoms of Type 1 diabetes include:
- Excessive Thirst: Known as polydipsia, individuals experience unquenchable thirst due to the body’s attempts to flush out excess glucose through urine.
- Frequent Urination: Polyuria results from the increased fluid intake and the kidneys’ efforts to eliminate excess glucose.
- Unexplained Weight Loss: Despite increased hunger and food consumption, individuals may lose weight as the body breaks down muscle and fat for energy.
- Fatigue: Ongoing high blood sugar levels can lead to constant fatigue and a lack of energy.
- Blurred Vision: Elevated blood sugar levels can temporarily affect the eyes, causing blurry vision.
Diagnosis
Blood Tests
Diagnosing Type 1 diabetes typically involves blood tests to measure blood sugar levels. Key diagnostic tests include:
- Fasting Blood Sugar Test: Measures blood sugar levels after an overnight fast.
- Oral Glucose Tolerance Test (OGTT): Involves fasting and then drinking a sugary solution to assess the body’s response to glucose.
- HbA1c Test: Reflects average blood sugar levels over the past two to three months.
Treatment and Management
Lifelong Insulin Therapy
Insulin Replacement: Managing Type 1 diabetes is primarily centered around insulin replacement therapy. Individuals with Type 1 diabetes must take insulin for life because their bodies do not produce any or produce very little insulin.
Types of Insulin: Various types of insulin are available, including rapid-acting, short-acting, intermediate-acting, and long-acting. Treatment plans may involve a combination of these to mimic the body’s natural insulin release.
Blood Sugar Monitoring
Frequent Testing: Regular monitoring of blood sugar levels is crucial for adjusting insulin doses and maintaining control.
Diet and Exercise
Balanced Diet: A balanced diet with controlled carbohydrate intake helps stabilize blood sugar levels.
Regular Exercise: Physical activity improves insulin sensitivity and can aid in managing blood sugar.
Complications
Long-Term Complications
Without proper management, Type 1 diabetes can lead to various long-term complications, including:
- Cardiovascular Disease: Increased risk of heart disease and stroke.
- Kidney Disease: Diabetes is a leading cause of kidney failure.
- Eye Problems: Damage to the blood vessels in the eyes can lead to vision impairment and blindness.
- Nerve Damage: Neuropathy can result in pain, tingling, and loss of sensation in extremities.
Type 1 diabetes is an autoimmune condition characterized by the destruction of insulin-producing beta cells in the pancreas. It requires lifelong insulin therapy, careful monitoring of blood sugar levels, a balanced diet, regular exercise, and ongoing medical attention. While there is no cure, with proper management, individuals with Type 1 diabetes can lead full and productive lives, reducing the risk of long-term complications.
For those affected by Type 1 diabetes, it’s essential to work closely with healthcare providers to create a personalized management plan and stay vigilant in monitoring and controlling blood sugar levels. Advances in diabetes research and treatment options continue to improve the quality of life for individuals living with Type 1 diabetes.
Type 2 Diabetes:
Introduction
Type 2 diabetes is a prevalent chronic metabolic disorder characterized by elevated blood sugar levels due to insulin resistance and inadequate insulin production. It is the most common form of diabetes, accounting for about 90-95% of all diabetes cases. This comprehensive guide will provide a detailed understanding of Type 2 diabetes, including its causes, risk factors, symptoms, diagnosis, management, complications, and prevention.
The Basics
Insulin and Glucose Regulation
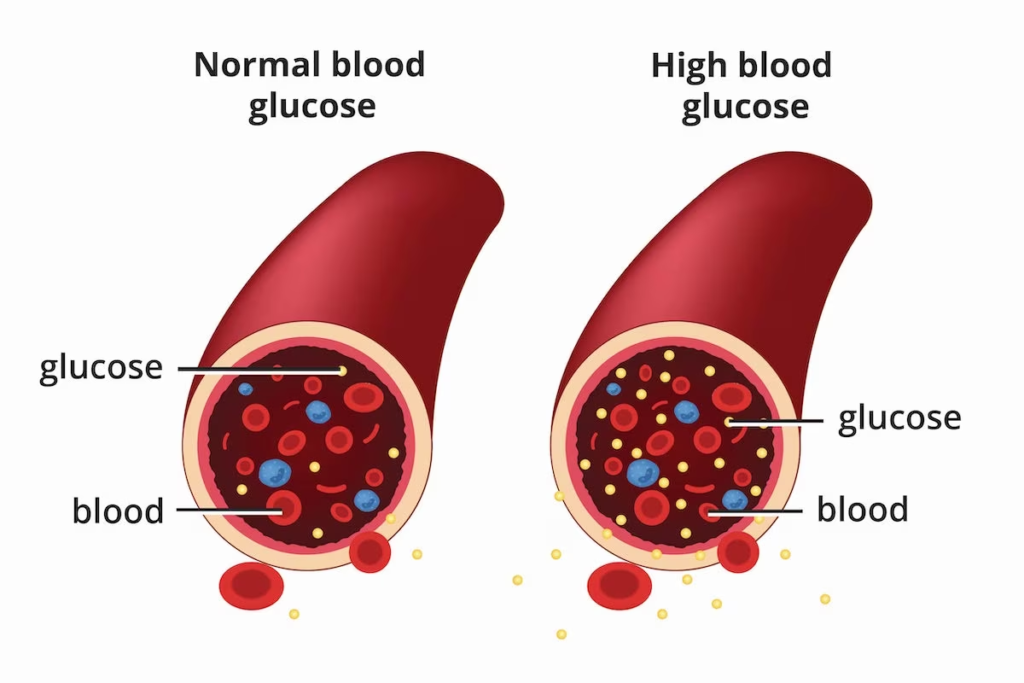
To understand Type 2 diabetes, it’s crucial to grasp the role of insulin. Insulin is a hormone produced by the pancreas, and its primary function is to regulate blood sugar (glucose) levels. After eating, the body breaks down carbohydrates into glucose, which enters the bloodstream. Insulin allows cells to absorb glucose for energy or storage. In Type 2 diabetes, this system becomes dysfunctional.
Causes of Type 2 Diabetes

Insulin Resistance
The hallmark of Type 2 diabetes is insulin resistance. This means that the body’s cells do not respond effectively to insulin, making it difficult for glucose to enter the cells. This leads to higher levels of glucose in the bloodstream, a condition known as hyperglycemia.
Inadequate Insulin Production
In addition to insulin resistance, many people with Type 2 diabetes also have reduced insulin production over time. The pancreas cannot keep up with the increased demand for insulin due to insulin resistance.
Risk Factors
Several risk factors increase the likelihood of developing Type 2 diabetes:
- Age: The risk increases with age, especially after 45.
- Family History: A family history of diabetes can increase your risk.
- Obesity: Excess body fat, particularly around the abdomen, is a significant risk factor.
- Physical Inactivity: A sedentary lifestyle contributes to insulin resistance.
- Poor Diet: Diets high in processed foods, sugary beverages, and low in fiber can increase the risk.
- Prediabetes: Having high blood sugar levels but not yet meeting the criteria for Type 2 diabetes.
- Ethnicity: Certain ethnic groups, including African American, Hispanic, Native American, and Asian American, have a higher risk.
Symptoms
Subtle Onset
Type 2 diabetes often develops gradually, and some individuals may not notice symptoms for years. Common symptoms include:
- Increased Thirst: Due to frequent urination.
- Frequent Urination: The body tries to eliminate excess glucose through urine.
- Unexplained Weight Loss: Despite increased appetite, weight loss can occur.
- Fatigue: Feeling tired or lacking energy.
- Blurred Vision: High blood sugar levels can affect the eyes.
Diagnosis
Blood Tests
Diagnosing Type 2 diabetes involves blood tests that measure blood sugar levels:
- Fasting Blood Sugar Test: Measures blood sugar levels after an overnight fast.
- Oral Glucose Tolerance Test (OGTT): Involves fasting and then drinking a sugary solution to assess the body’s response to glucose.
- HbA1c Test: Reflects average blood sugar levels over the past two to three months.
Management
Lifestyle Modifications
- Healthy Diet: A balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats helps control blood sugar levels.
- Regular Exercise: Physical activity improves insulin sensitivity and helps maintain a healthy weight.
- Weight Management: Losing excess weight can significantly improve blood sugar control.
Medications
- Oral Medications: Various medications can help lower blood sugar levels and improve insulin sensitivity.
- Injectable Medications: In some cases, injectable medications are prescribed when oral medications are insufficient.
Insulin Therapy
While not typically the first-line treatment for Type 2 diabetes, some individuals may eventually require insulin therapy to achieve adequate blood sugar control.
Complications
Long-Term Complications
Uncontrolled Type 2 diabetes can lead to various long-term complications, including:
- Cardiovascular Disease: Increased risk of heart disease, stroke, and hypertension.
- Kidney Disease: Diabetes is a leading cause of kidney failure.
- Eye Problems: Damage to the blood vessels in the eyes can lead to diabetic retinopathy and vision impairment.
- Nerve Damage: Neuropathy can result in pain, tingling, and loss of sensation in extremities.
Prevention
Type 2 diabetes is often preventable or delayable through the following strategies:
- Maintaining a Healthy Weight: Achieving and maintaining a healthy weight through diet and exercise can significantly reduce the risk.
- Eating a Balanced Diet: A diet rich in fiber, whole grains, and low in processed foods and added sugars is crucial.
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise per week.
- Routine Health Check-ups: Regular medical check-ups can help identify diabetes risk factors early.
- Avoiding Smoking and Excessive Alcohol: Both smoking and excessive alcohol consumption increase the risk of Type 2 diabetes.
Gestational Diabetes:

Introduction
Gestational diabetes is a specific form of diabetes that occurs during pregnancy. It affects about 2-10% of expectant mothers, making it a relatively common pregnancy-related health issue. Understanding the nuances of gestational diabetes is essential for expectant mothers, healthcare providers, and anyone interested in women’s health during pregnancy.
The Basics
Insulin and Blood Sugar Regulation
Like other forms of diabetes, gestational diabetes is rooted in insulin and blood sugar regulation. Insulin, produced by the pancreas, helps regulate blood sugar (glucose) levels in the body. During pregnancy, changes in hormones and the growing baby’s needs can affect this delicate balance.
Causes of Gestational Diabetes
Hormonal Changes
During pregnancy, the placenta produces hormones that can interfere with insulin’s action in the mother’s body. This condition is known as insulin resistance. As pregnancy progresses, the body must produce more insulin to keep blood sugar levels in check. In cases where the pancreas cannot produce enough insulin, gestational diabetes develops.
Risk Factors
Several factors increase the risk of developing gestational diabetes:
- Age: Women over the age of 25 are at higher risk.
- Family History: A family history of diabetes can increase susceptibility.
- Obesity: Excess weight before pregnancy increases the risk.
- Previous Gestational Diabetes: Women who had gestational diabetes in a previous pregnancy are more likely to have it again.
- Ethnicity: Some ethnic groups, including African American, Hispanic, Native American, and Asian American, have a higher risk.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS have a higher risk.
Symptoms
Usually Asymptomatic
Gestational diabetes typically does not cause noticeable symptoms in most cases. This is why routine screening during pregnancy is crucial.
Diagnosis
Screening and Testing
Gestational diabetes is diagnosed through screening and testing procedures:
- Glucose Challenge Test: This initial screening involves drinking a sugary solution, followed by a blood sugar test to determine how well the body processes glucose.
- Oral Glucose Tolerance Test (OGTT): If the glucose challenge test indicates potential issues, an OGTT may be conducted. It involves fasting overnight and then drinking a more concentrated sugary solution, with blood sugar levels measured at intervals.
Management
Lifestyle Modifications
The primary approach to managing gestational diabetes is through lifestyle modifications:
- Healthy Diet: A registered dietitian can help develop a meal plan that controls blood sugar levels while providing adequate nutrition for both the mother and baby.
- Regular Exercise: Physical activity can help lower blood sugar levels. Consult with a healthcare provider to determine safe exercise routines during pregnancy.
Blood Sugar Monitoring
Expectant mothers with gestational diabetes may need to monitor their blood sugar levels regularly to ensure they remain within a healthy range.
Medications
In some cases, lifestyle modifications alone may not be sufficient. Healthcare providers may prescribe insulin or oral medications to help manage blood sugar levels.
Complications
Potential Risks
While gestational diabetes is usually manageable, it can pose risks to both the mother and baby if not properly controlled. Potential complications may include:
- Large Birth Weight: High blood sugar levels can lead to excessive fetal growth, making delivery more complicated.
- Preterm Birth: Gestational diabetes increases the risk of premature birth.
- Low Blood Sugar in Newborns: After birth, babies born to mothers with gestational diabetes may experience low blood sugar levels.
- Preeclampsia: This condition characterized by high blood pressure and damage to other organs can be more common in women with gestational diabetes.
Post-Pregnancy
Continued Monitoring
After delivery, blood sugar levels typically return to normal. However, women who had gestational diabetes have an increased risk of developing Type 2 diabetes later in life. Regular check-ups and lifestyle modifications are crucial to preventing or managing Type 2 diabetes.
Conclusion:
In conclusion, diabetes is a complex and widespread group of metabolic disorders characterized by elevated blood sugar levels. There are different types of diabetes, with Type 1 and Type 2 being the most common, and gestational diabetes occurring during pregnancy. Here is a concise overview of what we’ve discussed about diabetes:
Type 1 Diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. It typically develops in childhood or early adulthood and requires lifelong insulin therapy.
Type 2 Diabetes is primarily characterized by insulin resistance, where the body’s cells do not respond effectively to insulin, and there is often inadequate insulin production. It is closely associated with lifestyle factors such as obesity, poor diet, and physical inactivity. It can often be managed or prevented through lifestyle changes and, in some cases, medication.
Gestational Diabetes occurs during pregnancy due to hormonal changes and insulin resistance. It typically does not produce noticeable symptoms but requires careful management through lifestyle modifications, blood sugar monitoring, and sometimes medications.
Key takeaways:
- Insulin plays a crucial role in regulating blood sugar levels.
- Genetics can contribute to the risk of developing diabetes, but lifestyle factors are equally important.
- Symptoms of diabetes can include increased thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision.
- Diagnosis is typically based on blood tests, including fasting blood sugar, oral glucose tolerance tests, and HbA1c measurements.
- Management involves lifestyle modifications, including a healthy diet and regular exercise, blood sugar monitoring, and medication or insulin therapy as needed.
- Complications of uncontrolled diabetes can include cardiovascular disease, kidney problems, eye issues, nerve damage, and more.
- Prevention focuses on maintaining a healthy weight, eating a balanced diet, regular physical activity, routine health check-ups, and avoiding smoking and excessive alcohol consumption.
Understanding diabetes, its causes, symptoms, and management strategies is crucial for individuals living with the condition, healthcare providers, and the broader community. Through education, proactive management, and healthy lifestyle choices, individuals can lead fulfilling lives while effectively managing diabetes and reducing the risk of complications. Regular medical check-ups and early intervention are key to ensuring the best possible outcomes for those living with diabetes.
